Why is it important?
When you hear the words evidence-based practice, you assume that means that a doctor, nurse or hospital follows proven treatments on providing the best care to you and everyone else. Is this true? What exactly is evidence-based practice? Does it provide a benefit or is it a made-up thing used by companies to profit?
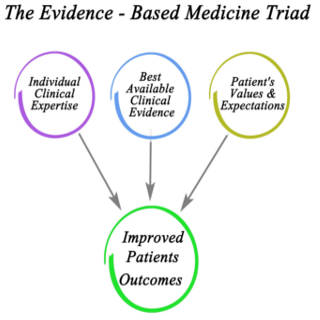 Evidence-based practice first came into concept in 1992 and has been gaining ground steadily since. It is supposed to be meticulous, clear, sensible and practical use of current, best evidence in guiding decisions about care of individual patients. It’s three parts are best available research, clinical expertise and patient values. Research is used to evaluate whether or not and why a treatment works. It is a systematic collection of data that is obtained through observation, experimentation, formulation of questions and testing of hypotheses. Clinical expertise is a combination of clinical judgment and experience of the clinician to identify the health state, diagnosis and risks/benefits of potential interventions for every person. Patient values refers to their beliefs and preferences in relation to medical treatment. The goal of combining these three items is to eliminate flawed or excessively risky practices in favor of those that yield better outcomes. Main undertaking of evidence-based practice is to replace single observations, rules or customs with practices that are based on data that has been rigorously collected and tested.
Evidence-based practice first came into concept in 1992 and has been gaining ground steadily since. It is supposed to be meticulous, clear, sensible and practical use of current, best evidence in guiding decisions about care of individual patients. It’s three parts are best available research, clinical expertise and patient values. Research is used to evaluate whether or not and why a treatment works. It is a systematic collection of data that is obtained through observation, experimentation, formulation of questions and testing of hypotheses. Clinical expertise is a combination of clinical judgment and experience of the clinician to identify the health state, diagnosis and risks/benefits of potential interventions for every person. Patient values refers to their beliefs and preferences in relation to medical treatment. The goal of combining these three items is to eliminate flawed or excessively risky practices in favor of those that yield better outcomes. Main undertaking of evidence-based practice is to replace single observations, rules or customs with practices that are based on data that has been rigorously collected and tested.
The benefits of EBP, when it is applied correctly, are extremely valuable. By having results from it, we can make better diagnoses. We can also use the evidence from treatment of previous individuals to help newly diagnosed people make more informed choices. In areas where we are lacking information, we can use this to devise research that will help to improve EBP. When we take the information that these studies provide us, we can use it to make widespread recommendations with more confidence. Supporters of EBP feel that these changes can help to address quality, cost and accessibility problems that occur in healthcare. The thought is that by using best practices that have come about from data and research, then it will reduce unnecessary care causing financial savings and offer pathways to people that produce improved results.
The problem with EBP is that some practices that are used as guidelines say that they are evidenced-based, but the evidence being used to support them are not appropriate to that practice. Unfortunately, these so-called “guidelines” are used by people and companies with an interest in them being popular in order for them to benefit. This is why some people criticize EBP because they associate it with weak guidelines and a way for companies and doctors to make more money by insisting that more medications and tests should be ordered. Some of these critics are from within the health profession. Insurance companies don’t feel that using EBP is an advantage because they feel that it places them on the hook to pay for certain treatments when there is minimal information to prove the value of doing so.
Regrettably, all of this mistrust of EBP is because we, as consumers of healthcare, treat all evidence as being equal. We need to understand that there is a difference between evidence that is statistically versus clinically significant. Statistically significant information can be achieved solely through having a larger enough group. This does not make it clinically significant and should not alter actual practice of those in healthcare. If studies do have clinically significant results, we need to be cautious before saying that it will work for everyone just because we have evidence that it worked. We have moved from concentrating on the disease to being concerned about risk. When something is dangerous to our health, we are quick to abandon using it without fully considering the extent of the risk associated with it or what we can do about it. In addition to the problem, we need to look at the solution. Just identifying as something being dangerous, doesn’t mean that it is necessarily dangerous for everyone or that a simple solution can not only make it safer but improve outcomes. The other key component of distrust of EBP is that we assume that all treatments are based upon sound evidence and if found not to work, a treatment is quickly abandoned. This is not true because uptake of medical evidence is slow and unsystematic. So, treatments enter in clinical practice before they are fully evaluated, doctors are poorly informed when treatments are ineffective and once a doctor starts using a treatment, it is challenging for them to stop. All of these lead to practices being used that aren’t necessarily based on sound evidence, getting infiltrated into the healthcare system and not being discontinued immediately upon discovery that it isn’t the best clinical practice.
Evidence-based practice can deliver numerous positive impacts, but it needs to be applied consistently and improved upon continually. The information needs to be provided in a clear and transparent manner to health care consumers and professionals so it can be used in a timely fashion that is most beneficial to patients. Evidence-based practice is a powerful tool that we can use to improve the quality of healthcare, but we need to do a better job of applying it appropriately.