Why is your leg swelling?
You’ve been sitting in the car on a long journey, when you get out of the car to go to the bathroom at the rest stop, you notice that your right calf is hurting. You don’t pay much attention to it, figuring it is stiff from being in the car. You go to the bathroom, get your snack and get back on the road. Later, once you’ve stopped driving for the day and get to your hotel for the night, now not only is your calf hurting, but it is swollen and red. What is going on? What is wrong with your leg?
 Definition
Definition
A deep vein thrombosis (DVT) is when a blood clot (thrombus) forms in one or multiple veins in your body. This can occur anywhere, but usually happens most often in your legs, especially your calves. It is caused by anything that prevents your blood from circulating or clotting normally. This can include, but not limited to, sitting for a long period of time, certain medical conditions or medications (they can affect your blood’s ability to clot), being overweight, having heart failure, smoking, being pregnant and being over the age of 60. The more risk factors that you have, the greater the chance that you might develop a DVT. The reason you are more likely to have a DVT in your calves is because your calf muscles help to circulate your blood from your legs back up to your heart as you move around. When your movement is limited for some reason, your blood is more likely to pool and clot. If you combine this with any of the other risk factors, you have an elevated likelihood of having DVT.
Sometimes, a DVT can occur without any symptoms, but usually most people have swelling in the affected leg with pain in the calf that feels like a cramp or soreness. Also, you may have redness or discoloration of your skin in the area. The areas will probably feel warm to the touch. If you notice that you have any of these symptoms, you should see your doctor. A concern with a DVT is that there’s a chance a portion of the clot could break off or the clot becomes dislodged and travels through your blood stream to your lungs blocking the blood flow there. This is known as a pulmonary embolism (PE) and is consider a life-threatening emergency. If you have signs of DVT and then have sudden shortness of breath, chest pain/discomfort that gets worse when you take a deep breath/cough, feel lightheaded/dizzy/pass out, rapid heart rate and/or cough up blood, then you should get medical treatment immediately.
Treatment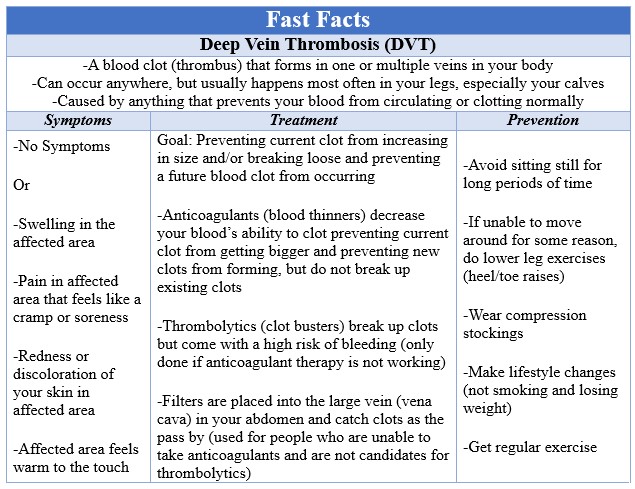
The number one goal of treatment of DVT is preventing the clot from increasing in size and/or breaking loose. The second goal is to prevent a future blood clot from occurring. The primary method to accomplish this is by using anticoagulants (blood thinners) to decrease your blood’s ability to clot. They usually come in the form of pills or injections that are given just beneath your skin. Typically, they are taken for at least 3 months depending on what your doctor says. They need be taken exactly as your doctor tells you. If you don’t take enough, you can have more clots form, but if you take too much, you could bleed too easily. Anticoagulants help prevent current clot from getting bigger and prevent new clots from forming, but do not break up existing clots. Thrombolytics (clot busters) are able to do this but come with a high risk of bleeding and only done if anticoagulant therapy is not working. It is usually done at a hospital not only due to the bleeding risk, but because the medicine is given intravenously (IV) or via a catheter that is placed directly near the clot. For people who are unable to take anticoagulants and are not candidates for thrombolytics, a filter can be placed into the large vein (vena cava) in your abdomen. This prevents blood clots from reaching your lungs by catching them as they travel in your bloodstream past the filter.
Prevention
In order to prevent a DVT, there are several things that you can do. The most important is to avoid sitting still for long periods of time. If you have just had surgery or are on bedrest, try to get moving as soon as your doctor will allow it. If you are sitting while working or relaxing, try not crossing your legs as this can impede blood flow. If you are traveling in a car, be sure to stop every hour to get out of the car and walk around. This is true if you are traveling by plane too. You should stand up and walk occasionally. If you are unable to move around for some reason, you can exercise your lower legs by doing heel raises followed by toe raises. This means keeping your toes on the ground and lifting your heels up and down. After doing several of those, switch and keep your heels on the ground and lift your toes up and down. These exercises engage the calf muscles and help improve blood flow through them. You could also wear compression stockings. They are long “sleeves” that start at your toes and usually come up to your knees and help prevent your blood from pooling in your calves. It is essential to make lifestyle changes, such as not smoking and losing weight, and getting regular exercise is crucial, especially for those who sit or travel often.
Having a DVT can come as a surprise and be a painful and scary experience when you consider the risk it creates for more serious complications. If you have any questions or concerns about having a DVT, please speak with your doctor. If you would like more information, please visit the Society for Vascular Surgery’s DVT page at https://vascular.org/patient-resources/vascular-conditions/deep-vein-thrombosis