What do you need to know?
When seeking medical help, did you know that as a patient you have certain rights that can and should not be infringed upon. Unfortunately, many of us are not aware of these rights and, therefore, do not even realize when a right has been denied. So, what are these rights? Are they an actual legal right or something that is generally followed as to what is an ethically appropriate thing to do?
 While there is no specific legal term known as “Patient Rights,” there are specific elements that are your legal right that when comprised together that experts equate to this. There are six main elements are deemed to be the main “rights” and they are in relation to consent, right to treatment, medical experimentation, advance medical directives, right to refuse care and privacy/confidentiality. Let’s take a closer look at each one of these.
While there is no specific legal term known as “Patient Rights,” there are specific elements that are your legal right that when comprised together that experts equate to this. There are six main elements are deemed to be the main “rights” and they are in relation to consent, right to treatment, medical experimentation, advance medical directives, right to refuse care and privacy/confidentiality. Let’s take a closer look at each one of these.
The first right is consent and this means that the patient gives approval for treatment. It must be voluntary, the patient must be informed and the patient must be competent to make any decisions (ex. they cannot be intoxicated). Consent can either be given verbally, in writing or by your actions, like waiting in line for a flu shot. Note, in emergent and life-threatening situations, consent is usually inferred in relation to preventing serious injury or death. A subset of this would be informed consent and means that the patient must be given basic information about what the doctor proposes to do before any treatment is provided. This should include a number of factors, such as the description of recommended treatment/procedure, description of benefits/risks (especially any risk for serious injury/death), alternative treatments with the benefits/risks of each of those, what is likely to occur if no treatment is taken, probability of success and what the doctor views success to mean, any challenges to/length of recuperation and any other information that is typically provided in the same situation by other qualified doctors.
The second right is the right to treatment. This means that a couple of things. In the first sense, it indicates that in an emergency situation, a person has the right to treatment regardless of the ability to pay. By emergency, this means that the situation is likely to cause serious injury/disability or death if not attended to promptly. Secondly, this means that a person cannot be refused treatment based on race, religion, national origin or has a specific disease, such as HIV/AIDS. Thirdly, this ensures that patients have the ability to refuse treatment at any point and leave against medical advice (the only time that this is not the case is if the person is determined to be mentally unsound and/or a danger to themselves or others).
The third right is in regards to medical experimentation. This means that a patient agreeing to participate in a medical experimentation m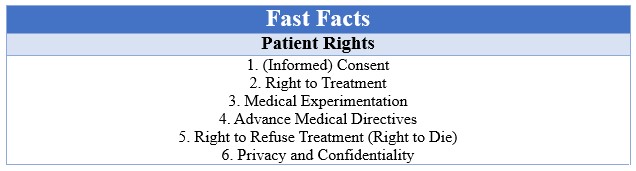 ust have given informed consent before beginning and can revoke it at any time. Just by agreeing to participate, does not mean the person surrenders any legal rights. It also means that all proper ethical, legal and moral concerns to prevent negligence must be followed by healthcare professionals because even with validly obtained consent it does not protect them from being sued if they don’t.
ust have given informed consent before beginning and can revoke it at any time. Just by agreeing to participate, does not mean the person surrenders any legal rights. It also means that all proper ethical, legal and moral concerns to prevent negligence must be followed by healthcare professionals because even with validly obtained consent it does not protect them from being sued if they don’t.
The fourth right is about advanced medical directives. Pretty much every state has some form of legislation related to advanced medical directives, but actual laws vary widely. Basically, they are documents that are made during a time when a person has full decision-making capabilities to be used to direct medical care when this capacity is lost. A living will is a type of advanced directive and usually specifies what a person wants or does not want in the case of life-threatening or debilitating illness. A durable power of attorney is a document where a person selects another person to perform certain acts or make certain decisions on the behalf of the first person. This can take place prior to or only after a person becomes incompetent to do so.
The fifth right is the right to refuse treatment (or right to die). Every person has the right to refuse life-sustaining medical treatments. Unfortunately, this particular right is featured a great deal in the news because it causes conflict between a patient’s autonomy, bodily integrity and privacy versus the traditional interests of preservation of life, prevention of suicide, protection of dependents and protection of the integrity of the medical profession.
The sixth, and final, right is concerning privacy and confidentiality. This means that a doctor is not allowed to disclose any information received from a patient to anyone who is not directly involved in that patient’s care. The reason this is so important is because it allows patients to feel comfortable sharing vital information with a doctor. This is key to the doctor’s ability to provide accurate treatment. There are only a few exceptions to this and they are birth and death certificates, child abuse must be reported, any infectious/contagious/communicable disease must be reported, in judicial processing or to notify a person to whom a patient may pose a danger.
With a deeper understanding of your rights, you are better prepared to receive the best quality care all healthcare settings. Healthcare professionals are advocates for patient rights, we encourage you to know what your rights are and we are willing to stand by your side to fight for what is right for you.